How to control blood sugar through diet?
With rising rates of diabetes and metabolic syndrome in the U.S., dietary management has become a cornerstone of blood sugar control. America’s diverse food culture and abundant choices present both challenges and opportunities for regulating glucose levels. By prioritizing nutrient-dense foods, optimizing meal composition, and avoiding processed sugars, individuals can achieve long-term stability without extreme restrictions. This article outlines actionable dietary strategies tailored to American lifestyles, focusing on ingredient selection, meal structuring, and habit formation.

I. Prioritize Low Glycemic Index (GI) Foods: Balancing Carbohydrates
The Glycemic Index (GI) measures how quickly foods raise blood sugar. Low-GI options slow glucose release, preventing spikes. Key choices in common U.S. diets include:
1. Whole Grains Over Refined Carbs
Replace white bread and rice with whole-grain alternatives like quinoa, brown rice, or oats. For example, whole-grain bread (GI ~50) has a significantly lower impact than white bread (GI ~75) and offers more fiber for sustained fullness. The USDA recommends at least half of daily grains be whole.
2. Fiber-Rich Vegetables and Legumes
Leafy greens (spinach, kale), cruciferous veggies (broccoli, cauliflower), and legumes (black beans, chickpeas) provide low-GI carbs alongside chromium and magnesium, which improve insulin sensitivity. One cup of cooked lentils contains ~40g of carbs and 18g of protein, making them an ideal carb substitute.
3. Smart Fruit Choices
Avoid tropical fruits (mango, pineapple) in favor of berries, apples (with skin), and citrus. A small apple (~95g) has 14g of sugar, but its pectin fiber slows sugar absorption by over 50% compared to juice.
II. Optimize Plate Composition: Protein and Healthy Fats Synergy
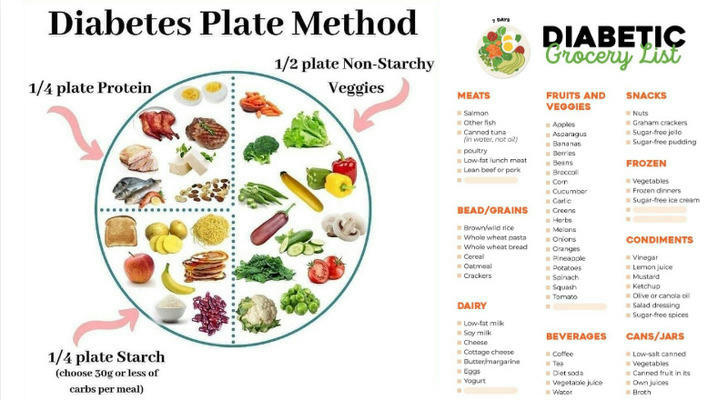
The typical American “large-portion, high-carb” meal often triggers post-meal glucose surges. Adjusting plate ratios can mitigate this.
1. Boost High-Quality Protein
Aim for 20–30g of protein per meal via chicken, turkey, fish (salmon, cod), or plant-based options (tofu, tempeh). Protein slows digestion and stimulates glucagon-like peptide-1 (GLP-1), aiding insulin release. A American Journal of Clinical Nutrition study found high-protein breakfasts reduced lunchtime glucose spikes by 20% in type 2 diabetics.
2. Swap Saturated Fats for Healthy Fats
Monounsaturated fats (olive oil, avocados) and omega-3s (walnuts, almonds) enhance insulin receptor function. Replace fries with avocado salad or use unsweetened almond butter instead of sugary spreads to flatten glucose curves.
3. Adopt the "Veggies First" Approach
Start meals with vegetables, followed by protein/fats, and finish with carbs. This sequence slows gastric emptying, smoothing glucose absorption. Trials show this method reduces post-meal spikes by ~30%.
III. Avoid Hidden Sugar Traps: Decoding U.S. Food Labels
Added sugars in processed foods are a major culprit in blood sugar dysregulation. Since 2021, FDA labels must list “Added Sugars,” empowering informed choices.
1. Spot Sugar Aliases
Ingredients like “brown rice syrup,” “fruit juice concentrate,” or “maltose” indicate added sugars. A 16-ounce “healthy” green tea bottle may contain 32g of added sugar—exceeding daily limits (25g for women, 36g for men).
2. Choose Low-Sugar Alternatives
• Opt for plain Greek yogurt over flavored versions (which can have 20g sugar per cup).
• Pick dark chocolate (70%+ cocoa) instead of milk chocolate, cutting sugar by ~60%.
• Flavor coffee or oatmeal with cinnamon or vanilla extract instead of syrup.
3. Beware of "Sugar-Free" Pitfalls
Some “sugar-free” products use sugar alcohols (maltitol, xylitol), which don’t spike glucose but may cause digestive distress if consumed beyond 50g daily.
IV. Adapting to American Lifestyles: Dining Out and Fast Food Hacks
Navigating fast food and convenience stores while managing blood sugar is possible with these tips:
1. Customize Fast Food Orders
• At Chipotle, opt for a bowl with lettuce instead of rice, double protein (chicken, steak), and guacamole.
• At McDonald’s, choose a grilled chicken sandwich (sauce-free) with a side salad instead of fries.
2. Convenience Store Solutions
• Build a protein-packed snack: low-sodium turkey slices (2oz) + mini cucumbers + cheese stick.
• Grab low-carb options: plain mixed nuts, hard-boiled eggs, or high-fiber bars (<5g added sugar).
3. Manage Social Drinking
Avoid sugary cocktails (margaritas, mojitos). Choose dry wine (5oz has ~4g sugar) or spirits (vodka, whiskey) with soda water and lime. Limit alcohol to twice weekly, as it may disrupt liver glucose production.
V. Tools and Habit Reinforcement: From Data to Action

Technology and behavioral strategies enhance adherence to sustainable dietary patterns.
1. Leverage Glucose Monitoring and Apps
Continuous glucose monitors (e.g., Freestyle Libre) reveal personal responses to foods. Pair with MyFitnessPal to track macros and refine meal plans.
2. Practice Mindful Eating
Avoid distractions (e.g., TV) while eating, and chew each bite 20+ times. Studies link mindful eating to 15% smaller glucose swings and reduced overeating.
3. Meal Prep for Success
• Batch-cook staples: roasted chicken, quinoa, pre-cut veggies for grab-and-go meals.
• Make low-sugar snacks: chia seed pudding (Greek yogurt + chia seeds + berries) as a dessert swap.
Conclusion
Managing blood sugar in the U.S. doesn’t require sacrificing culinary joy—it demands informed choices. From selecting low-GI staples to decoding labels, customizing fast food, and using tech tools, each step builds metabolic resilience. Sustainable glucose control lies not in rigid rules but in adaptable, culturally attuned habits that empower long-term health.