The Silent Pandemic: Antimicrobial Resistance (AMR) and What We Must Do
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, or parasites evolve to resist medicines designed to kill them. This makes infections harder to treat and increases the risk of severe illness or death. A 2024 study in The Lancet revealed that AMR directly caused 1.14 million deaths globally in 2021, with projections suggesting 10 million annual deaths by 2050 if no action is taken. While children under five have seen a 50% drop in AMR-related deaths since 1990, older adults (70+) face an 80% increase. This "silent pandemic" could undo decades of medical progress, making surgeries, cancer treatments, and even routine infections deadly again.
How Germs Outsmart Medicine: Simple Explanations
Natural Defenses of Microbes
Microbes develop resistance through genetic changes or by sharing resistance genes with each other. For example:
- Enzymes that destroy drugs: Bacteria like Klebsiella pneumoniae produce enzymes (e.g., carbapenemases) that break down antibiotics.
- Changing drug targets: Staphylococcus aureus (MRSA) alters its cell structure to avoid being targeted by methicillin.
- Pumping drugs out: Some bacteria use "efflux pumps" to eject antibiotics before they can work.
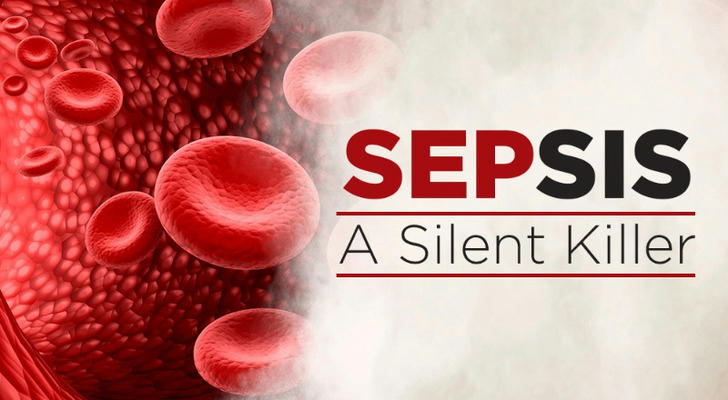
Human Actions Accelerate Resistance
Overusing antibiotics in humans and animals speeds up resistance. For instance:
- Healthcare misuse: Up to 50% of antibiotics prescribed in low-income countries are unnecessary.
- Farm animals: 73% of global antibiotics are used in livestock, promoting resistant strains that spread to humans through food and water.
- Environmental pollution: Antibiotics from factories and farms contaminate rivers, creating "hotspots" for resistance genes. In South Asia, 65% of rivers exceed safe antibiotic levels.
Key Threats: Deadly Pathogens and Infections
Sepsis: A Silent Killer
Sepsis, a life-threatening response to infection, is rising globally. Deaths surged from 14.1 million in 1990 to 21.4 million in 2021. While child sepsis deaths dropped by 60%, older adults now face double the risk due to weaker immune systems and chronic illnesses.
Superbugs to Watch
- Carbapenem-resistant bacteria: Acinetobacter and Klebsiella cause deadly hospital infections, with resistance to last-line antibiotics like carbapenems rising sharply.
- MRSA and TB: Methicillin-resistant Staphylococcus aureus (MRSA) and drug-resistant tuberculosis (TB) are spreading rapidly, especially in low-income regions.
- "Nightmare" Combinations: Resistance to multiple drugs (e.g., E. coli resistant to fluoroquinolones and cephalosporins) is becoming common.
Why AMR Is Everyone's Problem
Hospitals Under Pressure
Poor infection control in hospitals allows resistant germs to thrive. For example:
- MRSA infections: Cause 20% of surgical site infections in low-resource hospitals vs. 2-5% in high-income countries.
- Costs: Treating resistant infections costs 3-5 times more than standard treatments, straining healthcare budgets.
Food and Environment
- Contaminated food: Resistant bacteria from farm animals (e.g., salmonella) enter the food chain, causing outbreaks.
- Plastic pollution: Microplastics in water carry resistance genes, spreading AMR through ecosystems.
Global Travel and Trade
Resistant germs spread rapidly across borders. A 2025 report warned that air travel and food exports could make AMR uncontrollable without global cooperation.
Hope on the Horizon: Solutions in Action
Better Diagnosis and Treatment
- Rapid tests: CRISPR-based tools can detect resistant TB in 2 hours instead of weeks.
- New drugs:
- Zoliflodacin: A novel antibiotic targeting gonorrhea and other Gram-negative bacteria.
- Durlobactam: Combined with sulbactam, it fights multidrug-resistant Acinetobacter.
- Phage therapy: Viruses that infect and kill specific bacteria are being tested in clinical trials.
Preventing Infections
- Vaccines: Childhood vaccines (e.g., against Streptococcus pneumoniae) have cut AMR deaths by 60% in kids.
- Clean water and hygiene: Improving sanitation in low-income regions reduces infections and antibiotic use.
Global Cooperation
- One Health approach: The WHO, FAO, and UNEP collaborate to track AMR in humans, animals, and the environment.
- Norway reduced farm antibiotic use by 40% through stricter regulations and vaccines for livestock.
- Public campaigns: Vietnam's community education programs cut unnecessary antibiotic use by 35%.
What You Can Do: Simple Steps to Fight AMR
- Use antibiotics wisely: Only take them when prescribed, and finish the full course.
- Demand action: Support policies that limit antibiotic use in farming and fund research.
- Stay healthy: Vaccinations, handwashing, and safe food practices reduce infection risks.
The Road Ahead: Saving Lives Together
AMR is a complex crisis, but progress is possible. By 2050, improving healthcare access and developing 10 new antibiotics could prevent 92 million deaths. Key priorities include:
- Funding research: Only 12 of 97 drugs in development target critical pathogens.
- Global equity: Low-income countries need tools to track and treat resistant infections.
- Public awareness: Campaigns like World AMR Awareness Week (November 18-24) educate millions annually.
As the WHO warns, AMR is a "slow tsunami"—ignoring it risks returning to a time when a simple scrape could be fatal. Together, we can protect modern medicine and ensure antibiotics remain effective for future generations.